Lessons for the Next Pandemic
It might seem unthinkable today, but what would happen if another global pandemic occurred? After all, there's no guarantee that the Covid-19 outbreak will be the only such event in our lifetimes. So what have we learned? Will we be able to respond more effectively in the future?
The answers to these questions are not at all clear. In a time of deep division, most everyone agrees that the pandemic revealed a host of weaknesses in American society and in our public-health establishment's ability to handle deadly contagions. Yet the failures of 2020, 2021, and now 2022 provide some useful lessons.
In the future, we will almost certainly need to create better plans, develop additional tools, and deploy those tools more effectively than we have in the past two and a half years. And yet, as we have seen since March 2020, plans and tools are insufficient on their own. When a crisis strikes a representative democracy like ours, plans and tools also have to be deployed properly and in ways that the populace will accept.
Sadly, this effort has been made more difficult by the ugly politicization of nearly all aspects of the Covid-19 response. To do better next time, we will need to step back and look at what worked and what didn't without descending into the noisy lockdown, mask, and vaccine fights of the past few years. While some Americans have dug in to their respective political corners on these issues, the vast majority of the public wants solutions that work, regardless of which party is in charge. Rather than catering to those on the ideological extremes, policymakers should focus on keeping that vast middle engaged in the face of future pandemic threats.
THE MULTI-LAYERED DEFENSE
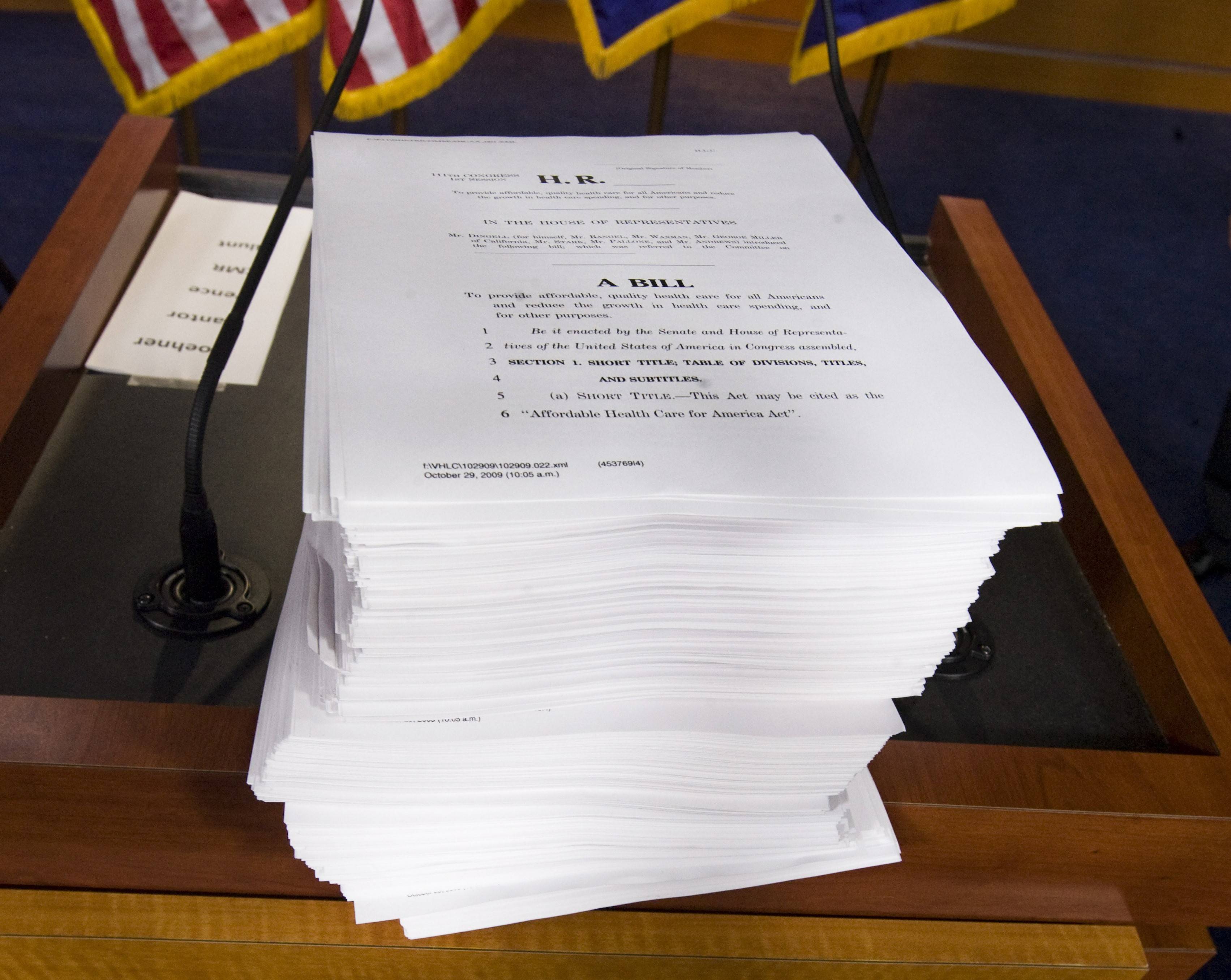
Some may find this surprising, but the United States did have a pandemic plan in place before 2020. The basic elements in the federal toolkit for pandemic response were developed in the early 2000s, largely as a result of President George W. Bush reading John Barry's best-selling book The Great Influenza. Accustomed to dealing with the unthinkable after September 11th, Bush decided that the United States should have a plan in place for any pandemic that emerges. (His subsequent request for $7 billion to address the influenza threat led congressional staffers to dub Barry's work "the seven-billion-dollar book.")
Bush and his team (on which I worked first as a senior White House policy staffer and then as deputy secretary of the Department of Health and Human Services) developed a multi-part pandemic strategy that included better monitoring of potential outbreaks, enhanced global-surveillance tools, better federal coordination with state and local health officials, more robust stockpiling of medical countermeasures for a wide array of pathogens, and, crucially, the development of three layers of defense against potential pandemic threats.
The first of these layers consisted of international monitoring. During the early years of the Bush administration, the Chinese government had prevented health experts from the United States and the World Health Organization (WHO) from learning the full extent of the Severe Acute Respiratory Syndrome (SARS) outbreak, which was first identified in China's Guangdong province. SARS ultimately sickened over 8,000 people and killed nearly 800, all while costing the global economy as much as $50 billion. In subsequent years, the international community had reason to believe that the Chinese government had learned its lesson from SARS and would be more cooperative in the future. The WHO also began working with both member and non-member states to develop regulations encouraging cooperation and disclosure when disease outbreaks occur.
The second layer of defense consisted of a testing regime that would allow public-health officials to test, track, trace, and isolate those who came down with a worrisome illness or may have been exposed to a given pathogen. The United States has deployed this approach effectively over the past two decades to limit the spread of diseases that have reached our shores. A prime example was the Ebola outbreak of 2014, which killed over 10,000 people in West Africa. Several cases did surface in America, but they didn't spread — in large part due to our system of modern infection controls and our ability to test, track, trace, and isolate individuals who came down with the illness.
The third layer of defense involved storing disease countermeasures in a Strategic National Stockpile (SNS). The SNS is an invaluable tool that can help the nation respond to a pandemic by transporting needed resources to any part of the country within 48 hours. In 2009, the United States used the stockpile to supply states with antivirals and protective equipment to combat the swine-flu epidemic.
Despite this multi-layered defense, our system did not prevent Covid-19 from entering America, nor did it keep the United States from underperforming most of the world in terms of restraining the pandemic's severity. As of this writing, our nation has endured the most Covid-19 cases and deaths of any country, while our deaths per capita have been more in line with those of Poland and Brazil than those of our typical comparators in Western Europe.
Such failures were the result of breakdowns in all three lines of our pandemic defense system. Despite our best hopes, in the early days of the outbreak China concealed what had happened in Wuhan, leaving the international health community largely in the dark as the novel coronavirus spread across the globe. Long after the pandemic materialized, China continued to obfuscate the virus's origin, which remains unknown. To this day, Chinese officials and state organs have persisted in their criticism of efforts to investigate the source of Covid-19.
In the early weeks of 2021, China and a WHO technical panel issued a joint report concluding that a scenario in which the virus had emerged from a Wuhan laboratory leak was "extremely unlikely." This may be the case, but even Tedros Adhanom Ghebreyesus — the WHO director general who has been accused of being too deferential to China — acknowledged that the report did not examine this possibility exhaustively. "Although the team has concluded that a laboratory leak is the least likely hypothesis," his statement read, it "requires further investigation, potentially with additional missions involving specialist experts."
As for our vaunted system of testing, tracking, tracing, and isolating cases, Covid-19 managed to evade it. To be sure, Covid-19 has characteristics that make it more difficult to constrain — it spreads more efficiently than Ebola, for example, and it can also spread asymptomatically, which makes identifying contagious patients more difficult. But these challenges were compounded by America's failure to develop an effective test for the virus during the initial stages of the pandemic. At the core of this problem was our national public-health agency: the Centers for Disease Control and Prevention (CDC).
Instead of adopting either the WHO's test for Covid-19, which it published in mid-January, or Thailand's test, which it released shortly thereafter, the CDC insisted that it could create its own, better test — something it failed to do for a month and a half. As the Washington Post would later write, "CDC leaders underestimated the threat posed by the new virus — and overestimated the agency's ability to design and rapidly manufacture a test." Meanwhile, the Food and Drug Administration (FDA), which served as the CDC's enforcer in the early days of the pandemic, directed labs working on their own tests to cease such efforts. As Yale University's Nicholas Christakis said of the botched testing rollout, "[i]f the country were a student in one of my courses, I would not hesitate to hand it an F."
This initial breakdown meant that the second layer of defense — testing, tracking, tracing, and isolating infected individuals — was not an option when the virus surfaced in the United States. Infected people were free to circulate at their own discretion, which posed a serious problem because Covid-19 spreads asymptomatically. Even today, America still lags in distributing affordable and reliable tests despite promises from elected officials to improve these capabilities.
With the first two layers of defense breached, we were left with one final layer: the SNS. When the pandemic began, however, the United States had neither a vaccine nor an effective antiviral for Covid-19. Ventilators — the rare available intervention — were in short supply, and were later shown to increase the risk of long-term hospitalization and death when used improperly. These shortcomings rendered the nation's stockpile effectively useless despite the billions of dollars the government had spent to develop and maintain it.
The absence of tools for dealing with a coronavirus outbreak was not only predictable, but predicted. As your author wrote in 2016:
One specific area that could stand improvement is the development of coronavirus countermeasures. Both MERS and SARS were worrisome pathogens, and the world lacked the countermeasures to combat them. Fortunately, science has advanced to the point where effective vaccine platforms will typically allow us to develop vaccines for new strains of an existing disease. With respect to flu, for example, we have the ability to develop new vaccines to inoculate against rapidly evolving new strains. With coronaviruses, we do not yet have those platforms.
While Covid-19 was a novel strain, the threat posed by a coronavirus outbreak was known to members of the pandemic-response community. The failure to prepare for such a possibility was a grievous mistake.
NON-PHARMACEUTICAL STOPGAPS
This failed opening was just the first act in what became a years-long, multi-act play. The first case of Covid-19 in the United States was confirmed in the state of Washington on January 20, 2020; by March 17, all 50 states had reported cases. Today — two and a half years after the virus first reached our shores — more than 80 million Americans have contracted the disease. Over 1 million of these individuals have died.
The pandemic's expansive reach and extended duration points to another misstep on the part of our public officials: the lack of planning beyond the initial outbreak. Before Covid-19, our nation's pandemic-response strategy had largely focused on how to prevent a deadly contagion from emerging in a discrete location. After those efforts failed, policymakers had insufficient plans for how to handle the spread.
Once it was clear that our first three lines of defense had failed, the next phase of the pandemic emerged: the period of non-pharmaceutical interventions, or NPIs. Lockdowns were the most obvious, the most intrusive, and perhaps the most controversial of the NPIs available. The Bush administration had included school closures, workplace social distancing, and cancelations of mass gatherings in its pandemic plans, but they were thought of as temporary and geographically limited measures. This is because lockdowns, as we have since learned, are unpopular, difficult to sustain, and have deleterious effects on the economy, children, and the poor. Back in 2009, when America was threatened with swine flu, then-president Barack Obama balked at pursuing even a social-distancing strategy because of the political challenges associated with it.
Nevertheless, for the first year of the Covid-19 pandemic (the period predating the vaccines), the primary NPI American governing officials deployed was the lockdown, which generally consisted of stay-at-home orders, business closures, and mandated social distancing. It remains unclear whether this approach was effective. The predominant view among media figures and the public-health community is that the lockdowns were necessary to avert even greater loss of life. Justin Lessler, an epidemiologist at the University of North Carolina, summarizes this view succinctly: "Lockdowns work, in the sense that extreme social-distancing measures stop transmission." "But," he acknowledged, "they're a short-term tactic."
This pro-lockdown position is hardly the only one, however. Stanford School of Medicine's Jay Bhattacharya has called the lockdowns the "biggest public health mistake we've ever made," characterizing the harm they caused as "catastrophic." In October 2020 Bhattacharya, along with Martin Kulldorff (formerly of Harvard University) and Sunetra Gupta of Oxford University, spearheaded the Great Barrington Declaration — a statement signed by 46 epidemiologists and public-health scientists expressing "grave concerns about the damaging physical and mental health impacts" of lockdown policies.
Regardless of one's position on lockdowns, the pushback against their use throughout the pandemic suggests they will remain controversial whenever they are considered. And while lockdowns can serve a purpose in responding to the initial outbreak of a novel pathogen, they are too flawed to serve as a viable long-term strategy for addressing pandemics.
To be sure, there were some attempts to limit the duration of the lockdowns — at least at the outset. In the early days of the outbreak, the Trump administration touted a "15 days to slow the spread" strategy. The idea behind this approach was to ensure that hospitals were not overwhelmed with patients, triggering a breakdown in the health-care system.
But as time passed, government and public-health officials repeatedly shifted the goalposts. "Fifteen days to slow the spread" soon turned into "30 days to slow the spread." Some states and municipalities locked down for months. It became clear to many that the intent behind the lockdowns was not to preserve scarce health-care resources, but to limit social and professional interactions indefinitely, or at least until a workable pharmaceutical intervention emerged.
The prospect of indefinite lockdowns was a daunting and frustrating one, especially as some areas, like New York, were being ravaged by the virus, while others, like Nebraska, were largely unaffected (at least at the time). The lockdowns also had a disproportionate impact on various populations: While white-collar office workers were largely able to continue their jobs remotely, those who couldn't work from home — retail cashiers, school-bus drivers, bartenders, barbers, and the like — had their work lives interrupted and their sources of income cut off. The stimulus programs alleviated these concerns to some degree, but they were temporary measures that were unsustainable in the long term.
Though the virus appeared to pose a reduced risk to the youngest Americans, they often suffered the brunt of the lockdown burden thanks to school closures. Children and adolescents were already experiencing a mental-health crisis in the years preceding 2020; pandemic restrictions only intensified matters. The increase in emergency-room visits for all mental-health troubles among young people during the pandemic — spurred by social isolation and other life disruptions — prompted three leading pediatric groups to declare a national state of emergency in the fall of 2021. And while remote learning offered a temporary solution to school closures, a recent working paper by the National Bureau of Economic Research found that student scores fell more sharply in areas where such methods were prevalent. These effects were especially pronounced among low-income and minority children.
As the pandemic wore on, the concept of "safetyism" — an extreme aversion to any kind of trade-off — took hold in many parts of the country, with the implicit goal (impossible as it was) being to ensure that no one contracted Covid-19. Then-governor Andrew Cuomo's statement — "if everything we do saves just one life, I'll be happy" — was paradigmatic of this attitude. But as a pandemic-fighting strategy, it was destined to fail.
THE COMMUNICATIONS CHALLENGE
While officials were quietly shifting the objective of the pandemic response, their mixed messages and partisan posturing muddied the waters further, making it difficult to put forth a coherent policy that Americans could adhere to.
From the beginning, President Donald Trump was ambivalent at best about the lockdowns. Though he issued travel restrictions in March 2020 and released guidelines urging people to avoid large social gatherings, he repeatedly tried to minimize the threat. "I wanted to always play it down," he told the Washington Post's Bob Woodward, "I still like playing it down, because I don't want to create a panic." He contradicted other members of his administration in public settings, and often appeared more concerned about how the lockdown measures affected his reelection prospects than their effectiveness at halting the virus's spread.
But public-health officials, who overwhelmingly favored the lockdowns, created additional problems by appearing callous toward their consequences, especially with regard to Americans living paycheck to paycheck. When people raised concerns, complained, or gathered to protest the economy-limiting measures, the condemnation from the public-health world and their Democratic supporters was swift and overwhelming. This was particularly the case with Michigan governor Gretchen Whitmer, who criticized residents for protesting the statewide stay-at-home order. Whitmer would go on to become not only the face of lockdowns, but of lockdown hypocrisy when her husband asked a boat contractor about launching his vessel for Memorial Day weekend following statements from Whitmer warning residents not to crowd the state's popular vacation spots.
This "lockdowns for thee but not for me" attitude would become a recurring problem among some Democratic politicians who staunchly advocated lockdowns for the public but did not always comply themselves. Some of the most prominent examples included House speaker Nancy Pelosi's visit to a hair salon and California governor Gavin Newsom's visit to an upscale restaurant when such activities were banned.
Another strain of lockdown hypocrisy emerged in the late spring of 2020, following the murder of George Floyd in Minneapolis. What began as legitimate outrage directed toward racial injustice snowballed into mass protests across the country, which contravened many states' restrictions on large gatherings. But instead of condemning these protestors, lockdown proponents praised them. New York City mayor Bill de Blasio went as far as exempting Black Lives Matter and related protests from his pandemic strictures, stating: "This is a historic moment of change. We have to respect that but also say to people the kinds of gatherings we're used to, the parades, the fairs — we just can't have that while we're focusing on health right now."
In these polarized times, it's perhaps not surprising that politicians would employ double standards when commenting on the public's behavior. A bigger surprise came on June 5, when a group released an open letter signed by over 1,200 public-health professionals that said of the racial-justice protests:
[A]s public health advocates, we do not condemn these gatherings as risky for COVID-19 transmission. We support them as vital to the national public health and to the threatened health specifically of Black people in the United States. We can show that support by facilitating safest protesting practices without detracting from demonstrators' ability to gather and demand change. This should not be confused with a permissive stance on all gatherings, particularly protests against stay-home orders.
The letter signaled to the public that certain activities — such as anti-lockdown protests — were worthy of condemnation, while others were permitted. This was a political distinction, not a scientific one. The inconsistency helped undermine the public's trust in the nation's leading health officials at a time when maintaining such trust was essential.
Masking became another unnecessarily controversial flashpoint due to messaging. To be sure, masks offered an imperfect solution at best, as non-medical-grade masks offer only modest protection to the wearer against Covid-19. Their real utility is in protecting others from one's own respiratory droplets — though even here, the research remains murky on how effective they can be.
Nonetheless, masks could have been a useful tool in the public's pandemic-response toolkit if officials had convinced the bulk of the population to wear them properly and consistently. But public-health leaders undercut their credibility when they actively discouraged the use of masks at the outset of the pandemic. This attitude was best illustrated by a late February 2020 tweet from Surgeon General Jerome Adams that read: "Seriously people- STOP BUYING MASKS! They are NOT effective in preventing general public from catching #Coronavirus, but if healthcare providers can't get them to care for sick patients, it puts them and our communities at risk!" Around the same time, Representative Chrissy Houlahan asked then-CDC director Robert Redfield, "should you wear a mask if you are healthy?" Redfield's answer was crystal clear: "No."
These statements sent the public the message that masks were ineffective — just as the first cases were emerging in the United States. Then, at the beginning of April, the message changed abruptly: The CDC began recommending that all Americans wear masks. What's more, the agency didn't limit the call to relatively narrow circumstances in which one is indoors with other people; instead, officials appeared to demand mask wearing in all circumstances outside the home. Stories abounded of people getting into altercations with those who failed to wear a mask in public, even outdoors. When schools reopened, many districts insisted on mask mandates for students despite there being little evidence that the virus severely harmed children.
As National Institute of Allergy and Infectious Diseases director Anthony Fauci would later acknowledge, the initial, anti-mask guidance was intentional: Officials wanted to discourage the American people from purchasing masks at a time when supply was low and front-line health-care workers needed them more urgently. But the about-face ended up compounding Americans' confusion: Some complied unquestioningly with the new guidance, while others felt the original hesitation must have been based on evidence that masks were useless.
Such turmoil was aggravated by President Trump, who objected to wearing masks in nearly all circumstances. At the April 3 press briefing where public-health officials announced the new masking guidance, Trump undercut the message by commenting, "it's voluntary; you don't have to do it. I don't think I'm going to be doing it." The president's persistent, and quite public, anti-mask biases only served to politicize the issue, with Republicans largely following Trump's lead and Democrats embracing a harder line on mask wearing.
The next area that led to confusion, and a further erosion of trust, occurred on the pharmaceutical front. As noted above, when Covid-19 struck, there were no pharmaceutical interventions available. The measures that were available — primarily ventilators — were of limited use. The absence of pharmaceutical interventions frustrated the American people, who tend to look for technological innovations as solutions to intractable problems.
This environment of distrust provided fertile ground for rumors of unconventional treatments like hydroxychloroquine, remdesivir, and monoclonal antibodies to proliferate. Hydroxychloroquine initially had some anecdotal evidence on its behalf, as well as some high-profile media figures pushing its use. But ultimately the data did not bear these predictions out. Remdesivir appeared somewhat more promising as a first-generation antiviral, though studies of its effectiveness have reached conflicting results. Monoclonal antibodies did ultimately prove effective, but they are expensive, not widely available, and have to be administered in the first few days of the illness's onset to be of any benefit.
These caveats notwithstanding, Trump loudly proclaimed the benefits of each treatment, appearing or claiming to have taken all of them when he was stricken with the virus in the fall of 2020. These declarations added to the confusion about which treatments might work. According to a study in the Journal of Medical Internet Research:
From March 1 to April 30, 2020, Donald J Trump made 11 tweets about unproven therapies and mentioned these therapies 65 times in White House briefings, especially touting hydroxychloroquine and chloroquine. These tweets had an impression reach of 300% above Donald J Trump's average....Google searches and purchases increased following his first press conference on March 19, 2020, and increased again following his tweets on March 21, 2020. The same is true for medications on Amazon, with purchases for medicine substitutes, such as hydroxychloroquine, increasing by 200%.
Trump's praising of these therapies (and his later apparent use of them as treatments) led to increased interest in them among the public. Compounding matters was the fact that the near unanimous opposition to Trump from the public-health community made it seem as if the president's celebration of potential therapies made public-health experts all the more eager to debunk them. When the various treatments did not pan out, the public-health world appeared to express more glee than sorrow.
All this would have long-term implications in raising doubts about public-health officials' pronouncements regarding vaccines — something we are still dealing with today. As with lockdowns and masks, there were multiple bad actors.
Trump was one: He saw the issue in political terms and wanted the vaccine available by the November 2020 election. Standard FDA guidelines require monitoring clinical-trial participants for at least two months before an emergency approval can be sought, and when the FDA refused to speed up the timeline in October, it became clear there was no chance the vaccine would be ready before the election. In light of the announcement, Trump reportedly told his Health and Human Services secretary, Alex Azar, "[w]e need a vaccine before the election, and this guidance is going to delay that." The spat between the White House and the FDA went public, and even though the administration followed the latter's approach, the perception of political gamesmanship over the vaccine raised questions about its safety and efficacy.
Yet Trump was not the only one to inject politics into the issue. On October 7, then-vice-presidential candidate Kamala Harris said in her debate with Vice President Mike Pence: "If the public health professionals, if Dr. Fauci, if the doctors tell us that we should take it, I'll be the first in line to take it — absolutely. But if Donald Trump tells us that we should take it, I'm not taking it." She was not alone. Other Democratic politicians, including Joe Biden, Governor Cuomo, and Representative Ilhan Omar made public statements raising questions about the vaccine while the Trump administration was still in office.
After Biden defeated Trump in November, it would be Republicans who raised questions about the vaccine — often in the context of objecting to vaccine mandates. Representative Marjorie Taylor Greene tweeted that the "vaccines are failing and do not reduce the spread of the virus," while Representative Madison Cawthorn tweeted, "Big Pharma gets BILLIONS in taxpayer dollars. And what do we get in return? A vaccine with no guarantees." It's doubtful that they would have made such comments had Republicans maintained control of the White House. What both sides seemed to forget was that vaccines belong to neither party. A change in political leadership should not bring about a change in one's views about a vaccine.
When it comes to disasters, the chief resource the government has at its disposal is public trust. The lockdown hypocrisy, the about-face on masking, the confusion over therapies, and the politicization of masks and vaccines undermined this trust. Americans need more than reassurance in a crisis situation; they need direction and conviction from their leaders. What they received instead was inconsistency and partisan bickering.
WHAT WENT RIGHT
Amid all this failure, there were some bright spots in America's pandemic response that are worth considering.
Perhaps foremost among them is how the United States eventually mobilized to develop a series of successful vaccines. Operation Warp Speed not only helped fund their development, it also guaranteed purchases of vaccines even if they did not pan out, thereby incentivizing development and production. The vaccines that resulted were both remarkably safe and effective at reducing the virus's severity. And despite some hiccups, approximately 75% of our nation's adult population had received at least one dose of a vaccine by the end of 2021, while 85% of its seniors were fully vaccinated.
These numbers are more impressive when one realizes that the United States reached these levels by the end of December 2021 when even the most optimistic predictions suggested there might not be a vaccine until 2022. Furthermore, this was the first widespread application of mRNA technology, which could lead to other life-saving vaccines in the future. Discovering how to develop mRNA vaccines quickly after establishing the sequencing of a pathogen has put us closer to being able to deploy a platform approach to fighting contagions. If successful, the SNS will no longer have to rely on narrowly tailored countermeasures that work only if our pandemic planners make correct predictions regarding future pathogens.
Another silver lining of the pandemic was revealed in the work of our doctors and other front-line health-care workers. Amid a crisis, they experimented, innovated, and shared improved techniques with other doctors in other hospitals. Social media, for all its many faults, gave medical workers the ability to communicate new and effective treatment ideas directly with one another. As Mount Sinai nurse Valerie Burgos-Kneeland told the Wall Street Journal, "[i]f it wasn't for all the social media and technology, we'd all be living in silos."
Modern technology also brought with it another blessing: the infrastructure enabling many Americans to work from home and entertain themselves there. Broadband internet, streaming services, Zoom, cell phones, and the entire technological revolution — much of which has only existed since around 2010 — made it much easier for the bulk of the populace to endure a long period of social and professional isolation. In the spring of 2020, about 35% of the labor force was able to work from home — a percentage that likely rose as more workplaces made adjustments to deal with the ongoing pandemic. Obviously there were still many more employees — including many at the lower end of the income scale — who could not work from home. Still, the large percentage of those who could lessened the pressure on productivity, made downtown areas less crowded, and reduced the possibility of spread on public transportation.
Technology also helped calm a restive population. According to the Pew Research Center, 93% of Americans use the internet, and approximately three-quarters of Americans have broadband internet at home. Fifteen percent of U.S. adults may not have home access to broadband, but they do have access to the internet via smartphone. This meant that the vast majority of the population could access entertainment, receive news and other updates, order food, and stay in touch with friends and relatives electronically. There were certainly moments of unrest during the pandemic, but for the most part, the U.S. population was remarkably calm during an unusually trying time. The widespread availability of recent innovations in technology helped make that relative tranquility possible.
Finally, there were our governing institutions. For all the talk of division and the inability to get anything done in Washington, the truth is that Congress stepped up, in an overwhelming and bipartisan way, during the early stages of the crisis. The $2 trillion relief package passed in March of 2020 helped keep the economy and the citizenry afloat as Americans adjusted to a new reality. And it did so with relatively little partisan rancor. One can certainly quibble with many of Congress's subsequent actions (including its decision to maintain these programs to the point where they created a disincentive to return to the workforce), but the initial passage of the CARES Act showed that Congress can still get things done at moments of great need.
In sum, as the American Enterprise Institute's Hal Brands has observed, America's response to Covid-19 "fits within the historical pattern of U.S. responses to major challenges: agonizingly slow starts, as was also the case in World War I and World War II, followed by dramatic, war-winning surges." So despite many of its pandemic-response failures, Americans ultimately got many of the big things right.
WHAT WE STILL NEED TO FIX
Of course, there is still vast room for improvement. The breakdown of our nation's three layers of defense at the pandemic's outset, along with what occurred afterward, teaches us several lessons about how we should approach future pandemics.
First, and most obviously, we need to bolster those three initial layers of defense. This includes more robust monitoring by U.S. public-health and intelligence agencies of emerging contagions in other parts of the world. The United States should also adopt a more skeptical stance toward disease reporting from authoritarian governments.
During the Covid-19 pandemic, both the CDC and the FDA made it more difficult for the private sector to develop tests in a timely manner, leading the United States to lag behind other industrialized nations on that front. Going forward, the CDC needs to be willing to call on private entities and university research labs to lend their expertise to this endeavor. Likewise, the FDA needs to encourage, rather than discourage, non-CDC actors that try to develop tests of their own, and update its outdated submission guidelines for new tests.
More broadly, we need to make sure that our public-health agencies maintain increased focus on their primary mission: the prevention of deadly communicable diseases. When Covid-19 emerged, public-health agencies' focus had drifted, as if pandemic threats were a thing of the past. Instead, officials tended to prioritize behavioral modification, or convincing Americans to give up harmful habits and adopt healthier lifestyles. Former FDA commissioner Scott Gottlieb made this point in a 2021 interview, observing that over time, the CDC has "evolved much more towards a disease prevention mission — reducing heart disease, smoking cessation — and away from its core disease control" mission. Meanwhile, the portion of the CDC's work that people have a more romantic view of — officials raiding hot zones in hazmat suits and extracting samples to analyze in a lab — "has been subordinated to the...policy aspects of the CDC's mission." While harmful and potentially costly, personal choices are not communicable, nor do they have the same capacity to disrupt our society as do contagious pathogens. Our public-health agencies should prioritize the latter.
It will not be easy to convince a whole generation of public-health officials who have devoted their careers to behavior modification to focus on rapid pandemic response. Public-health agencies also tend to be resistant to political interference, so asking Congress to lead the charge is unlikely to generate the changes needed within CDC as it exists today. One way to help mitigate this problem could be to create a separate agency solely focused on the pandemic threat, with no brief to expand its operations to behavior modification. Such a restructuring would also address the issue of no one appearing to be in charge when a pandemic occurs. To ensure that this pathogen-focused agency stays true to its mission, it would have to be subject to political oversight — joint reporting to both the Department of Health and Human Services and the White House could help in that regard. The failure of our response to Covid-19 could make this a propitious moment for such a reform.
We also need to invest more — and more wisely — in the SNS to ensure that it can anticipate and respond to pandemic threats. In addition to pharmaceutical countermeasures, the SNS stores masks, gloves, hospital gowns, and ventilators — all of which were in short supply when the pandemic hit. The shortage occurred in large part because the SNS distributed some of its stockpile during the swine-flu outbreak of 2009 but did not replenish it.
The purpose of a national stockpile is to have these materials on hand in case of an emergency; it does little good if they are not available when the country needs them. Going forward, the SNS needs to stay fully stocked, and to replenish its coffers following deployments.
The SNS should also take advantage of the new vaccine-platform technologies to refine and perfect its rapid-response capabilities. Over time, such technology will allow us to develop the right countermeasures for a given virus, as opposed to stockpiling assets that are effective only if planners have the right ones on hand for whatever pathogen happens to emerge.
On the NPI front, we need to rethink our lockdown strategy. While lockdowns were one of the few tools available when the first three layers of defense broke down, they should never be deployed again on a nationwide scale. With better data and testing, we can determine where and to what extent such efforts are necessary and deploy them in a more targeted and strategic manner.
Officials also need to reconsider their approach to messaging. During crises, Americans naturally look to their leaders for guidance. Misleading the American people, even for a worthy cause, is a dangerous maneuver that can — and did — have serious negative consequences. Once leaders deliberately deceive Americans, it erodes public trust in authority. Public-health officials need people to follow their directives in order to effectively combat a pandemic. This is a more difficult ask when the public is skeptical of the sincerity or accuracy of those directives, or when leaders fail to offer a unified front.
To avoid squandering their initial stock of public trust, officials must be forthright about the nature of the crisis, the seriousness of potential threats, the limitations of government capabilities, and the concomitant responsibility of the citizenry. They must work to maintain a reasonable degree of consistency, and when disagreements arise (as they inevitably will), our leaders should avoid highlighting them in public settings. Finally, officials should work to keep politicization at a minimum: Injecting partisan politics into the fray raises doubts and diminishes credibility, thereby weakening the government's ability to encourage citizens to take its directives seriously.
With regard to masks in particular, it was undoubtedly true that frontline health-care workers desperately needed masks — especially medical-grade masks — at the outset of the pandemic. It's also true that a run on masks would have made it harder for hospitals to secure enough masks for their workers. But instead of misleading the American people, public-health leaders could have been candid about the scarcity of medical-grade masks and asked the public not to hoard those, while at the same time suggesting that cloth masks could be a potential alternative for non-health-care workers.
These requests could have come with a call directed toward one of America's greatest assets: the industriousness and ingenuity of its people. Throughout the Covid-19 ordeal, we witnessed a classically American mobilization response to shortages in a variety of areas, including hand sanitizer, face shields, and, eventually, masks themselves. With an honest assessment of the situation and request for assistance from the public, that mobilization effort could have begun sooner.
Officials should also be wary of the temptation to embrace safetyism. Every public-policy decision involves costs and benefits, and disaster response requires some of the most challenging trade-offs of all. A response based on safetyism, which rejects the notion of trade-offs on principle, leads to paralysis and poor choices. Planners need to expunge this pernicious sensibility from their calculations.
Finally — and insufficiently discussed among policymakers thus far — is the matter of planning for the various stages of a pandemic. U.S. pandemic planning before Covid-19 focused mainly on the first stage, in which the three layers of defense were to be deployed to prevent a pandemic from taking hold. What we discovered was that there are multiple phases that take place during a pandemic, each of which requires different political responses.
After the initial stage, in which we failed to contain the virus, there was a second stage — the realization that we had only NPIs to combat the virus. A third stage emerged once the vaccine was ready but we had insufficient doses, followed by a fourth stage in which we had plenty of vaccine doses available but insufficient take-up among the population. Then came a fifth stage, during which the surge of the Delta variant indicated a return to the more wary behavior of the second stage. And Delta had not even fully receded before the Omicron variant arose, bringing a more infectious, yet apparently less deadly, variant into the mix.
Of course, every pandemic is different, and there will never be a comprehensive manual telling policymakers exactly what will happen or how to respond. But advance planning that tailors different strategies to different stages can give policymakers more guidance and make policymaking less haphazard as a virus mutates and our toolkit evolves.
In the future, it should not be stopgaps and safetyism that drive our policy, but a strong public-health system with multiple — and well-maintained — layers of defense that keep us protected from deadly pandemics. Public-policy messaging should remain consistent throughout, albeit with a recognition that different stages of the pandemic will require different interventions by policymakers and different behaviors from the affected population. The debate over the effectiveness of Covid-19 policies will continue in perpetuity, but a proper biodefense strategy, effectively implemented, should generate better results.